Related Articles
 Jan 08, 2025
Jan 08, 2025
Is Varicose Vein surgery covered under the health insurance policy in India
 Health Insurance
Health Insurance
The Insurance Regulatory and Development Authority of India (IRDAI) is a statutory body formed under an Act of Parliament for the overall development and supervision of the Insurance sector in the country. Every year IRDA publishes the Incurred Claim Ratio (ICR) and Claim Settlement Ratio (CSR) of health insurance companies. Read on to learn more about IRDA and CSR in this post.
The Insurance Regulatory and Development Authority of India (IRDAI) is an apex body that governs the workings of the life and non-life insurance companies operating in the market.
Every insurance company is required to follow the rules and guidelines laid down by the IRDAI. IRDA also publishes regular reports on the performance of insurance companies. The amount of business done by insurers, their claim settlement ratios, incurred claim ratios, etc. are computed and published by IRDA regularly. Amongst these publications, the claim settlement ratio of insurance companies is very widely used.
Let’s understand what this is.
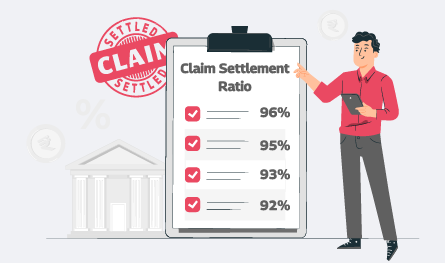
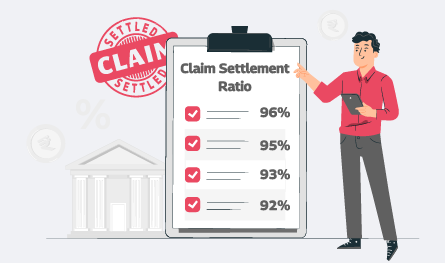
Claim settlement ratio (CSR) in health insurance is the ratio between the total number of claims received by an insurance company and the number of claims that were settled by the insurer from among the ones received in a particular financial year. This ratio ensures that the insurer is capable of settling claims of its customers.
For instance, suppose in a particular financial year, 100 claims were filed by different policyholders of an insurance company. However, the insurer settles 97 out of the 100 claims. In that case, the CSR of the health insurance company for the particular year would be 97%.
The formula to calculate claim settlement ratio of health insurance companies = (total claims settled/total claims filed) * 100
The ICR or Incurred Claim Ratio calculates the ratio between the total number of claims that are paid by a health insurance company to customers as compared to the total amount collected by the company in premiums in a particular financial year. For example, an insurer with an 88% claim ratio would signify that the company has paid INR 88 in claims for every INR 100 earned as premiums. Thus, the extra INR 12 is the profit earned by the company.
The IRDAI or the Insurance Regulatory and Development Authority of India publishes the ICR or the incurred claim ratio of different insurance companies every year. Along with the ICR of the health insurance company, IRDAI also offers specific ICRs for various forms of insurance for the customers to check at the time of buying a policy. So, customers can check the annual report of IRDAI to estimate the ICR of health insurance companies.
The claim settlement ratio of an insurance company measures the proportionate claims which the company has settled from the total number of claims made on it in a financial year. The ratio is calculated using the following formula -
Health Insurance Claim Settlement Ratio = (total claims paid by the company / total claims made on it) * 100
The ratio is expressed as a percentage. Higher the percentage the better are the chances of the claims being settled by the insurance company.
IRDA also publishes the claim settlement ratio and incurred claim ratio of health insurance companies. The ratios are calculated and published at the end of each financial year. The ratio shows policyholders the probability of their health insurance claims being settled.
Since health insurance policies are important and have also become quite popular, a potential customer can judge the performance of a health insurance company based on the claim settlement ratio published by the IRDA. This makes choosing the health insurance company easy. It helps customers make informed choices.
There are more than twenty health insurance companies in the insurance market. Comparing and selecting the best insurer, therefore, becomes quite difficult. However, with IRDA’s health insurance claim settlement ratios, this comparison becomes easy. Individuals can choose a company after choosing the best health insurance plan and then comparing the claim settlement ratios.
Below are some points that show the importance of the CSR in health insurance:
| Health Insurance Company | Claim Settlement Ratio 2022-23 | Cashless Hospitals |
| Care Health Insurance Company | 95% | 9,592 |
| Niva Bupa (formerly known as Max Bupa) Health Insurance Company | 96% | 8,701 |
| Star Health Insurance Company | 90% | 11,035 |
| Aditya Birla Health Insurance Company | 94% | 8,787 |
| DIGIT Health Insurance Company | 96% | 5,479 |
| Reliance Health Insurance Company | 100% | 8,014 |
| Royal Sundaram Health Insurance Company | 89% | 8,332 |
| Oriental Health Insurance Company | 89% | 2,716 |
| Liberty Health Insurance Company | 94% | 5,552 |
| Future Generali Health Insurance Company | 92% | 6,303 |
Below are the Claim Settlement Ratios of insurance companies in India:
| Health Insurance Company | Claim Settlement Ratio (2021-22) |
| Care Health Insurance Ltd. | 100 |
| Aditya Birla Health Insurance Co. Ltd | 99.41 |
| Acko General Insurance Ltd | 97.2 |
| Bajaj Allianz General Insurance Co. Ltd | 96.59 |
| Go Digit General Insurance Ltd. | 96.09 |
| HDFC ERGO General Insurance Co. Ltd. | 98.49 |
| ICICI Lombard General Insurance Co. Ltd. | 97.07 |
| ManipalCigna Health Insurance Co. Ltd. | 99.9 |
| Niva Bupa Insurance Company | 99.99 |
| SBI General Insurance Co. Ltd. | 95.04 |
| Star Health and Allied Insurance Co. Ltd. | 99.06 |
| United India Insurance Co. Ltd. | 97.25 |
The claim settlement of health insurance companies takes place in two ways. They are the cashless claim process and the reimbursement claim process.
Cashless Claim Process – Cashless claims are filed when a policyholder avails treatment at a network hospital of the health insurance company. Here are the steps to file the claim:
Reimbursement Claim Process – These claims are filed when the policyholder chooses a non-network hospital to get treatment. Here, the policyholder has to pay the hospital bill from his/her pocket at the time of discharge and later can submit the claim of reimbursement to the health insurance company. Here are the steps to follow:
Below are the documents required:
You can check the IRDA health insurance claim settlement ratio of companies by the below process:
Make a list of the CSRs of different health companies and compare them to check the company with a high claim settlement ratio. Buy the best plan from the best company with the best CSR.
Claim Settlement Ratio (CSR) is the ratio of the total number of claims settled by an insurance company against the total number of claims that the company receives for processing for a financial year.
Claim Settlement Ratio (CSR) is the ratio of the total number of claims settled by an insurance company against the total number of claims that the company receives for processing for a financial year. The CSR customers to identify the ability of an insurance company to meet claim requests. A ratio above 80% is generally considered as a good claim settlement ratio in health insurance.
Health insurance companies in India in the year 2022-23 with best Claim Settlement Ratio are:
IFFCO Tokio General Insurance (96.57%)
Magma HDI (96.41%)
New India Assurance (95.92%)
(Source - IBAI Claims Insight Handbook 5th Addition)
The top health insurance companies on the basis of Claim Settlement Ratio (CSR) are:
IFFCO Tokio health insurance
Aditya Birla Health Insurance
Bajaj Allianz Health Insurance
Tata AIG Health Insurance
Bharti AXA Health Insurance
Care Health Insurance
United India Health Insurance
Universal Sompo Health Insurance
SBI Health Insurance
The formula to calculate health insurance claim ratio is:
Incurred Claim Ratio = Net claims incurred / Net Premiums collected.
Thus, health insurance claim ratio is the overall value of total claims that insurance company has paid divided by the total sum of premium collected during the same period.
Insurance claims might get rejected if the information offered is wrong or if you miss to add any information. Thus, wrong information is the most common factor for claims getting rejected. This is because personal information such as age of the insured, profession of the insured, his/her health condition as well as medical history etc. determines the premium and risk coverage of a health insurance policy.
It is not compulsory to always find the best claim settlement ratio of health insurance companies to buy a plan from. However, the CSR of a company does prove to be a deciding factor in selecting an insurer.
You can check the IRDAI website for the IRDAI health insurance claim settlement ratio.
IRDAI instructs health insurance companies to settle claims in 30 days.
India has more than 20 private insurance companies providing insurance. Some of them are:
- Bajaj Allianz General Insurance Co. Ltd.
- Cholamandalam MS General Insurance Co. Ltd.
- Future Generali India Insurance C. Ltd.
- Go Digit General Insurance Ltd.
- HDFC ERGO General Insurance Co. Ltd.
- ICICI Lombard General Insurance Co. Ltd.
- IFFCO Tokio General Insurance Co. Ltd.
- Kotak Mahindra General Insurance Co. Ltd.
- Liberty General Insurance Ltd.
- Royal Sundaram General Insurance Co. Ltd.
- SBI General Insurance Co. Ltd.
- Tata AIG General Insurance Co. Ltd.
- Universal Sompo General Insurance Co. Ltd.
- Aditya Birla Health Insurance Co. Ltd.
- Care Health Insurance Ltd.
- ManipalCigna Health Insurance Co. Ltd.
- Niva Bupa Health Insurance Co. Ltd.
- Star Health and Allied Insurance Co. Ltd.
There are over 7 standalone health insurance companies functioning in India, namely;
- Aditya Birla Health Insurance Co. Ltd.
- Care Health Insurance Ltd.
- HDFC ERGO Health Insurance Co. Ltd.
- ManipalCigna Health Insurance Co. Ltd.
- Niva Bupa Health Insurance Co. Ltd.
- Reliance Health Insurance Ltd.
- Star Health and Allied Insurance Co. Ltd.
Yes, there some over 4 public sector health insurance companies functioning in India, namely;
- National Insurance Co. Ltd.
- The New India Assurance Co. Ltd.
- The Oriental Insurance Co. Ltd.
- United India Insurance Co. Ltd.
Information on CSR is available on the official website of IRDAI or the Insurance Regulatory and Development Authority. Every year, IRDAI publishes annual reports with information on the CSR of every Health insurer in the country.
80% and above is considered a good CSR in health insurance.
Young and healthy? Find out which of these plans rewards you with lower premiums. Click here to check now!

Paybima Team
Paybima is an Indian insurance aggregator on a mission to make insurance simple for people. Paybima is the Digital arm of the already established and trusted Mahindra Insurance Brokers Ltd., a reputed name in the insurance broking industry with 21 years of experience. Paybima promises you the easy-to-access online platform to buy insurance policies, and also extend their unrelented assistance with all your policy related queries and services.

.jpg)
Having a bike is not just about convenience, it’s a huge responsibility. Financial protection of your two-wheeler is important and the best way to ensure that is to have a bike insurance policy that will protect you in case of an accident, theft or a natural calamity. There are so many options when it comes to policies, making it difficult to know what’s best. This guide makes it easier to choose the best bike insurance policy that is suitable for you.


Non-linked, non-participating term plans are the ones that do not participate in the business and profit of the insurance company. These are fixed premium plans where the policyholder pays a fixed amount to ascertain a guaranteed sum as a return to be paid to the nominee in case of his/ her demise. Let’s learn more in this post.

Car depreciation implies the difference between the cost of a car at the time of buying the car and when you sell it. A car insurance claim amount is determined by the car depreciation rate. The car depreciation rate is the reduction in the value of your car over its lifespan caused by wear and tear.


Have you ever caught yourself lost in illusions about your daughter's future events, such as her university convocation and first day at work? Her university convocation. When she embarks upon her initial job after graduation will be the day.

.png)
Accidents can happen anywhere, anytime, by your own fault or another person. What’s important is to be prepared for such mishaps. This is where Own Damage Car Insurance comes in handy.
